RADIUS: Die Erweiterung Ihrer therapeutischen Reichweite!
Sie behandeln Abhängigkeitserkrankungen und arbeiten nach dem Community Reinforcement Approach (CRA). Wie unterstützen Sie Ihre Klienten zwischen den Sitzungen?
Was ist RADIUS?
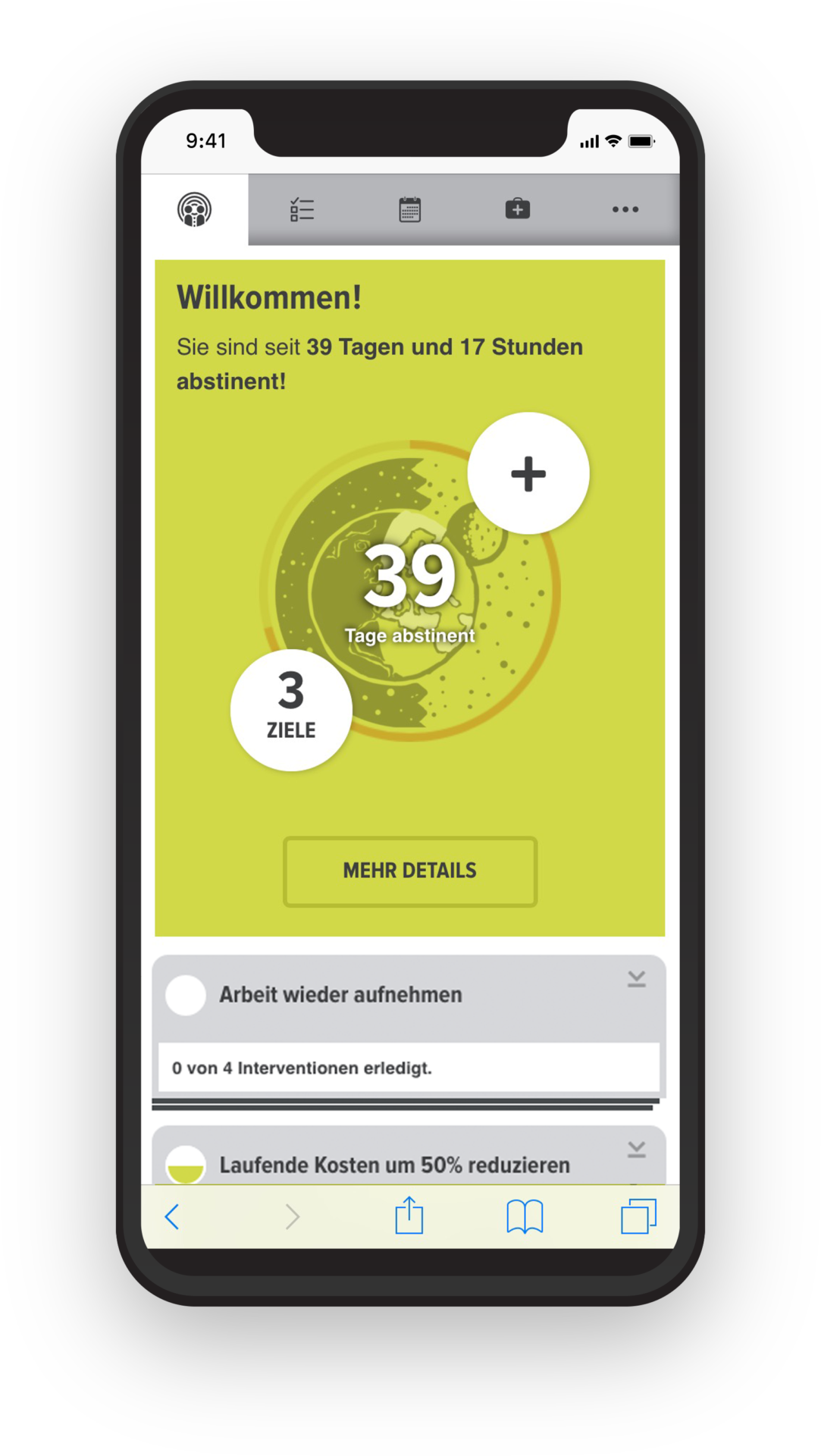
Die einzige internetbasierte Therapieunterstützung speziell für die Behandlung von Abhängigkeitserkrankungen nach dem Community Reinforcement Approach (CRA).
Wenn Sie nach den Ansätzen der Gemeindeorientierten Therapie arbeiten, dann erreichen Sie dank RADIUS Ihre Klienten mitten in deren Lebensalltag auch auf dem digitalen Weg. Die internetbasierte Schnittstelle unterstützt dabei alle Beteiligten:
Hilfe für Klienten
- optimale Integration von CRA in den Alltag
- Hilfestellung auch zwischen den Sitzungen
- persönliche Motivation und Aktivierung
Hilfe für CRA Counselor
- zentrale Abbildung und Verwaltung der individuellen Behandlungspläne
- grafische Mustererkennung des Verhaltens zwischen den Sitzungen
- sichere Kommunikationsschnittstelle zu den Klienten
Sehen sie hier welche Funktionen RADIUS im Detail enthält und wie Sie davon in Ihrer Therapie profitieren können.
Was sagen CRA Experten über RADIUS?
„Der Communty Reinforcement Approach ist alltags- und ressourcenorientiert, der begleitende Profi oft eher ein Coach als ein Therapeut. RADIUS hilft uns als Online-Arm unseres netzwerkorientierten Behandlungsansatzes, den Kontakt zu den Klienten in deren Alltag hinein zu halten. RADIUS ist deswegen als eines der „Kinder“ des CRA Modells ein wichtiger Beitrag zu einer innovativen zukunftsorientierten Suchtbehandlung, die sich an den individuellen Bedürfnissen der Nutzer orientiert.“
Dr. Martin Reker
CRA Ausbilder und Supervisor
Ltd. Arzt der Abt. Abhängigkeitserkrankungen
Klinik für Psychiatrie und Psychotherapie, Bethel
Wir können Ihnen viel erzählen, testen Sie lieber selbst!
Richten Sie sich einen kostenlosen Testzugang für RADIUS ein und erleben Sie den vollen Funktionsumfang so lange Sie möchten. Erkennen Sie die Vorteile für den behandelnden Counselor in der Übersicht aller seiner Klienten. Loggen Sie sich ein als Klient und erleben Sie die nahtlose Integration in den Alltag auf dem Handy.

Sie möchten RADIUS gern an Ihrer Einrichtung einsetzen?
Geben Sie uns einen kurzen Hinweis und wir stellen Ihnen Ihr persönliches Angebot zusammen:
